Duodenal Switch Surgery in Rancho Cucamonga
Lasting weight loss through biliopancreatic diversion
Duodenal switch is a bariatric surgery procedure that can achieve dramatic weight loss and improve or reverse obesity-related health problems. This advanced procedure reduces stomach size, reroutes the small intestines, and removes the gall bladder to help patients lose weight rapidly and feel less hungry every day. Best of all, a duodenal switch achieves permanent changes to help you keep the weight off long-term.
This advanced procedure is performed only by select, specially trained surgeons nationwide, and our experienced weight loss surgeons at Surgical Arts of the Inland Empire are proud to offer it to patients in Rancho Cucamonga.
Duodenal switch is weight-loss surgery designed to treat people who have severe obesity.
Benefits of a duodenal switch
- Permanently reduces stomach volume to physically restrict food intake
- Intestinal rerouting helps the body absorb fewer calories
- Helps reduce feelings of hunger
- Patients experience rapid weight loss (studies show an average loss of 70% of excess weight within 1 year)
- Lower rate of weight regain compared to some other bariatric procedures for weight loss
- Can significantly alleviate or reverse obesity-related conditions, such as diabetes, sleep apnea, asthma, non-alcoholic fatty liver disease, cardiovascular disease, and joint pain
- Has a high long-term success rate
How is the duodenal switch procedure performed?
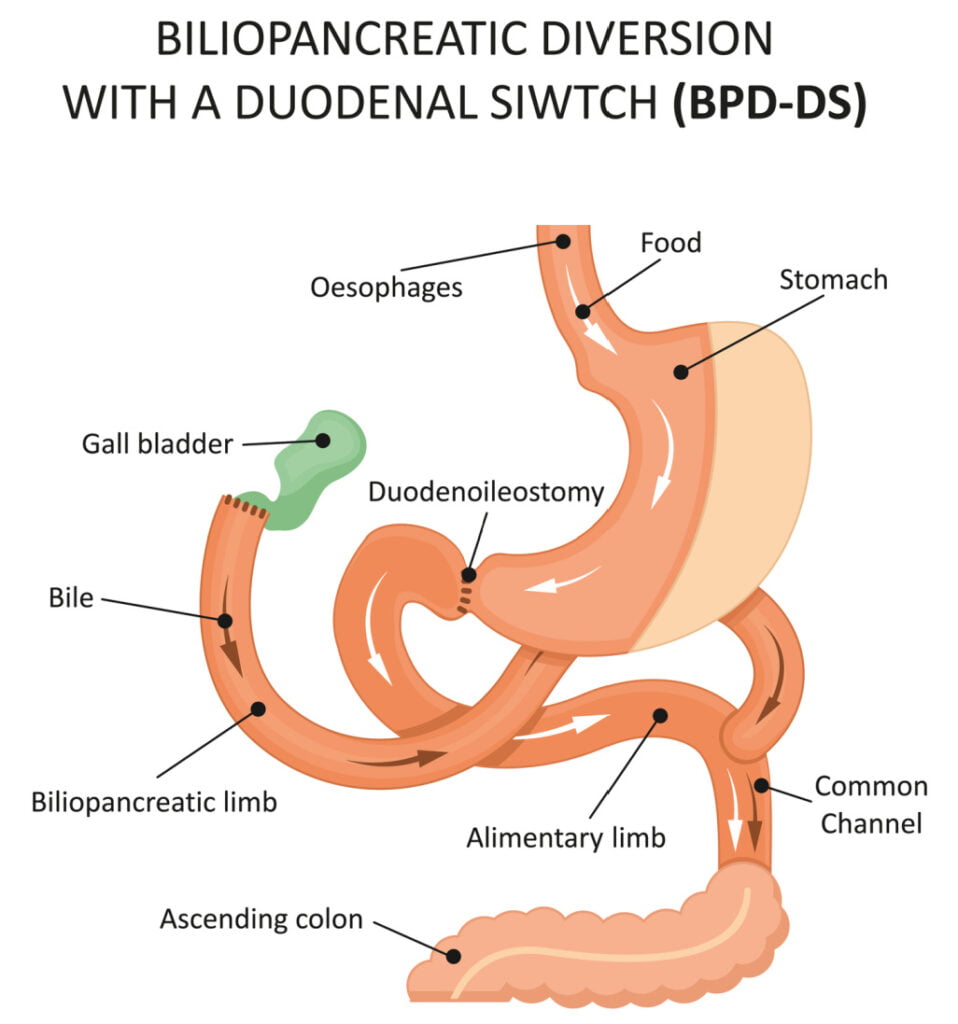
Duodenal switch surgery is performed laparoscopically (using small, thin instruments placed through several small incisions). This two-step surgery first begins with a gastric sleeve, or an operation to reduce stomach size by up to 80%. This reduces the amount of food you can eat at any given time, helping you take in fewer calories.
Next, the upper portion of the small intestine (a.k.a. the duodenum) is detached and rerouted to connect at a lower point. This step helps your body absorb fewer calories as it digests your food, as well as intensifies the release of hormones that signal the “fullness” feeling.
Finally, in most cases, the gallbladder is removed during the same operation. This reduces the output of digestive juices and prevents your body from absorbing as many fats or other nutrients.
Surgery and recovery information
This is a complex procedure that can take several hours to complete. General anesthesia is used for your safety and comfort, and a 2 to 3-day inpatient stay is required to monitor your early recovery. Patients typically need 2 to 3 weeks away from work and 4 to 6 weeks to recover fully. You will be on a heavily restricted diet for several weeks and will need to take nutritional supplements for life to prevent deficiencies.
Am I a good candidate for duodenal switch?
Duodenal switch surgery can be a good option for patients who are currently considered morbidly obese (BMI of 40 or higher), or obese patients who are currently experiencing health problems such as sleep apnea, diabetes, or hypertension. Our surgeons can help you determine if this procedure is a safe, suitable option for you based on your:
- Current weight and BMI (this procedure is meant for those whose BMIs put them in the category of having morbid obesity)
- Past attempts to lose weight through traditional means
- Medical history-patients with certain conditions such as GERD or inflammatory bowel disease may not be good candidates for duodenal switch
- Mental health and ability to commit to permanent lifestyle changes. Like any bariatric surgery, duodenal switch requires patients to modify their eating patterns for life in order to ensure optimal nutrition and prevent weight regain.
- Key Benefits
- Glossary
- Typically results in substantial long-term weight loss by reducing the stomach size and altering the digestive process
- Improves or resolves obesity-related conditions, including type 2 diabetes, high blood pressure, sleep apnea, and dyslipidemia
- Enhances feelings of fullness and reduces hunger, aiding in weight management
- Decreases the absorption of fats, thus aiding in weight loss and reducing calorie intake
- Lower risk of developing gastric ulcers, especially if patients avoid smoking and NSAID use
- High rates of sustained long-term weight loss among bariatric procedures
- Absorption: The process by which nutrients from food are taken into the body.
- Bariatric Surgery: Surgical procedures aimed at weight reduction for individuals with obesity. These include the Duodenal Switch, gastric bypass, gastric sleeve, and gastric banding.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): A complex weight-loss surgery that involves removing a portion of the stomach and rerouting the small intestine to limit food intake and nutrient absorption.
- Body Mass Index (BMI): A measure used to classify obesity based on height and weight. A BMI of 30 or higher is considered obese, with higher values indicating more severe obesity.
- Comorbid Conditions: Health issues that often occur alongside obesity, such as type 2 diabetes, hypertension, sleep apnea, and heart disease, which can improve or resolve after bariatric surgery.
- Duodenal Switch (DS): See Biliopancreatic Diversion with Duodenal Switch.
- Duodenum: The first part of the small intestine. It connects to the stomach. During this two step surgery, the duodenum is detached and rerouted to connect at a lower point.
- Gastric Bypass: A type of bariatric surgery that creates a small stomach pouch and reroutes the small intestine, promoting significant weight loss and hormonal changes that affect hunger and satiety.
- Gastric Sleeve (Sleeve Gastrectomy): A surgical procedure that removes a large portion of the stomach, leaving a tube-shaped “sleeve,” reducing the amount of food that can be consumed.
- Malabsorption: A reduced ability to absorb nutrients from food, intentionally created by some bariatric surgeries like the Duodenal Switch, contributing to weight loss.
- Nutritional Deficiencies: The state of lacking essential nutrients, which can occur after bariatric surgeries, especially those causing malabsorption, requiring lifelong supplementation.
- Obesity: A medical condition characterized by excessive body fat accumulation, posing significant health risks. Bariatric surgery is an option for individuals with severe obesity when other treatments have failed.
- Pyloric Valve: The valve controlling food movement from the stomach to the small intestine. Preserving this valve in the DS helps prevent dumping syndrome and maintains a more natural digestion process.
- Satiety: The feeling of fullness or satisfaction from eating. Bariatric surgeries, including the DS, often enhance satiety earlier during meals, helping to reduce overall calorie intake.
- Semaglutide: A injectable weight loss medication approved for weight loss and diabetes management that mimics an intestinal hormone to reduce appetite; not directly related to duodenal switch surgery but part of broader weight management strategies, and is a non-surgical alternative.
- Staple Line: The surgical seam created by stapling the stomach or intestine during bariatric procedures. Proper healing of the staple line is crucial to prevent leaks.
- Weight Loss Plateau: A common phase in the weight loss journey where the patient temporarily stops losing weight, often addressable through dietary and lifestyle adjustments.
- Weight Loss Surgeon: A medical specialist who performs surgical procedures aimed at aiding weight loss, typically for patients with severe obesity.
What are the risks of this procedure?
While duodenal switch surgery has a high success rate and a lower complication rate than some other bariatric surgery options, there are risks and long-term side effects associated with this procedure that you should be aware of:
- General anesthesia risks
- Rare chance for bleeding, staple line leaks, intestinal perforation, or strictures
- Nutritional deficiency
- Nausea, vomiting, and/or indigestion when eating certain foods
- Increased risk of bone fractures
- Sagging skin following rapid weight loss
- Gallstone formation
You can minimize more serious risks by choosing an experienced, qualified surgeon for your procedure and following your doctor’s instructions regarding recovery, diet, and nutritional supplementation after surgery. Remember, success with weight loss requires a long-term commitment. Additionally, it’s important to consider the long-term health risks of remaining obese when thinking about your weight loss surgery options. At Surgical Arts of Inland Empire, our weight loss surgeons are here to help. Schedule a consultation to find out whether duodenal switch surgery, or another one of our bariatric services, is right to help you reach your health and wellness goals.
To learn more about duodenal switch and discuss whether you are a good candidate, contact Surgical Arts of Inland Empire.References »
American Society for Metabolic and Bariatric Surgery. Bariatric Surgery Procedures (https://asmbs.org/patients/bariatric-surgery-procedures). Accessed 5/3/2024.
Anny Aasprang, John Roger Andersen, Villy Våge, Ronette Kolotkin, Gerd Karin Natvig. Ten-year changes in health-related quality of life after biliopancreatic diversion with duodenal switch. Surgery for Obesity and Related Diseases, Volume 12, Issue 8, 2016, Pages 1594-1600, ISSN 1550-7289, https://doi.org/10.1016/j.soard.2016.04.030.
Anthone GJ, Lord RV, DeMeester TR, Crookes PF. The duodenal switch operation for the treatment of morbid obesity. Ann Surg. 2003 Oct;238(4):618-27; discussion 627-8. doi: 10.1097/01.sla.0000090941.61296.8f. PMID: 14530733; PMCID: PMC1360120.
Kapeluto JE, Tchernof A, Masckauchan D, Biron S, Marceau S, Hould FS, Lebel S, Lescelleur O, Julien F, Biertho L. Ten-year remission rates in insulin-treated type 2 diabetes after biliopancreatic diversion with duodenal switch. Surg Obes Relat Dis. 2020 Nov;16(11):1701-1712. doi: 10.1016/j.soard.2020.06.052. Epub 2020 Jul 7. PMID: 32800734.
Marceau P, Biron S, Hould FS, Lebel S, Marceau S, Lescelleur O, Biertho L, Simard S. Duodenal switch: long-term results. Obes Surg. 2007 Nov;17(11):1421-30. doi: 10.1007/s11695-008-9435-9. PMID: 18219767.

