Weight Loss Surgery is Most Effective For Long-Term Blood Pressure Control

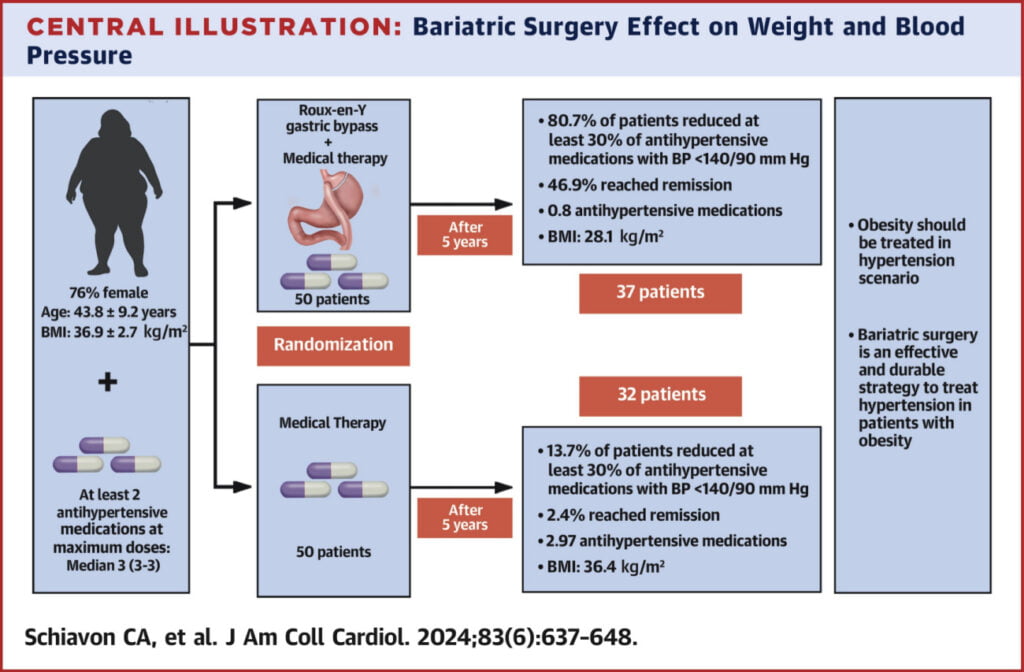
A 5-year study by the American College of Cardiology found that compared to blood pressure medications alone, weight loss surgery maintains blood pressure with fewer medications and lowers Body Mass Index (BMI) in people with obesity and uncontrolled high blood pressure.
First published in February 2024 in the Journal of the American College of Cardiology, the study investigated the impact of treating obesity in order to lower high blood pressure. Their reasoning: while promising new medications, such as semaglutide injections, are regularly introduced to treat obesity, sticking to these kinds of weight loss medications over long periods can be difficult, for both physical and financial reasons. So the researchers looked at bariatric surgery as a long-term solution to control high blood pressure.
The study
The researchers studied 100 people aged 18 to 65 (76 of 100 were female) with grade 1 or grade 2 obesity. All participants had hypertension and were actively using at least two blood pressure medications at the time of the study.
The study excluded people with a history of cardiovascular issues (such as a heart attack) and people with poorly controlled Type 2 diabetes.
The subjects were split into two groups: participants in one group underwent Roux-en-Y gastric bypass surgery in addition to taking medication; the other group continued to take their medications without bariatric surgery.
The results
Results were assessed five years later and were quite promising. At five years, the researchers evaluated changes in the two groups relating to their BMI, any reduction in their medications, and hypertension remission (when a person achieves controlled blood pressure without medication).
BMI results:
- Bariatric surgery group: 28.01 Kg/m² average BMI
- Medication-only group: 36.40 Kg/m² average BMI
Medication reduction:
- Bariatric surgery group: 80.7% reduction in medication use
- Medication-only group: 13.7% reduction in medication use
Hypertension remission rates:
- Bariatric surgery group: 46.9% achieved hypertension remission
- Medication-only group: 2.4% achieved hypertension remission
In this new study, researchers assessed the potential of treating obesity as a long-term solution for lowering high blood pressure.
What you need to know about bariatric surgery for lowering high blood pressure
These results highlight the effectiveness of addressing hypertension by first treating obesity. The 5-year outcome suggests that pairing gastric bypass surgery with medication offers greater long-term benefits in BMI reduction, fewer medications, and even hypertension remission compared to people who rely on blood pressure medication alone.
While this is promising, it’s worth noting that further research is needed. This study involved a small sample size, and participants underwent a specific type of bariatric surgery. Whether other weight loss surgery methods prove to be as effective is yet to be determined. Additional research on different medications would also be helpful in determining the “ideal” treatment for those who are obese and have high blood pressure.
About Surgical Arts of Inland Empire
We understand that health and wellness are incredibly individualized, which is why our expert weight loss surgical staff works with you to create personalized treatment plans to help you establish lasting, healthy habits. If you are struggling with your weight and are considering help from a qualified medical professional, contact us online or call (909) 579-3111 to schedule your weight loss consultation today.
References »
American College of Cardiology. “Weight loss surgery most effective for long-term blood pressure control.” ScienceDaily. ScienceDaily, 5 February 2024. <www.sciencedaily.com/releases/2024/02/240205165757.htm>.
Carlos A. Schiavon, Alexandre B. Cavalcanti, Juliana D. Oliveira, et al. Randomized Trial of Effect of Bariatric Surgery on Blood Pressure After 5 Years. Journal of the American College of Cardiology, Volume 83, Issue 6. 2024. https://doi.org/10.1016/j.jacc.2023.11.032.
